Struggling before your period? Take our science-based PMDD quiz and guide to understand your symptoms and find support.


Period Pill × 3mbrace Health
I show up strong. I get things done. I laugh. I love. And then something shifts.
Rage out of nowhere. Tears I can’t explain. A heavy fog in my brain. And deep in my body, an ache that words can’t quite touch.
And just as suddenly, it’s gone.
If you feel like a different person before your period, this isn’t your imagination. It could be PMDD, a hormone-based mood disorder that affects roughly 5-8% of menstruating individuals.
This guide and quiz are here to change that.
Premenstrual Dysphoric Disorder (PMDD) is a condition that causes extreme mood changes and physical symptoms in the second half of the menstrual cycle, typically in the two weeks before your period starts. Once menstruation begins, these symptoms usually fade quickly.
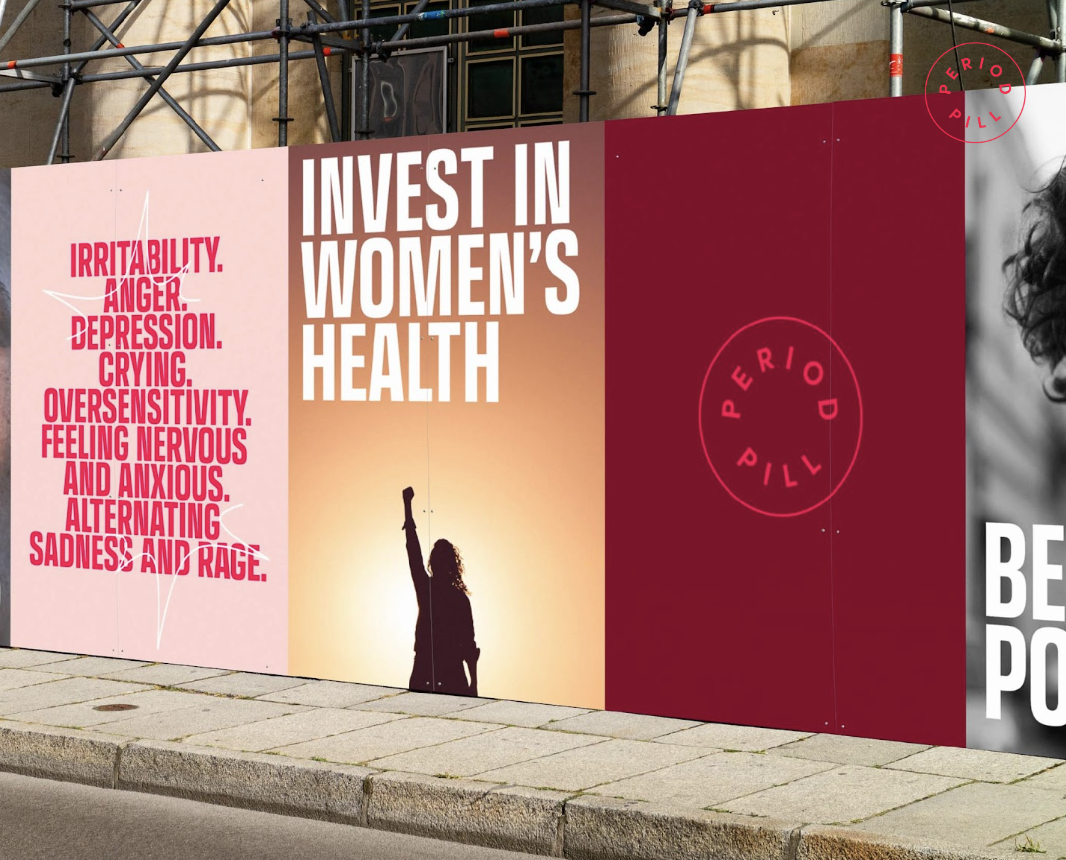
People with PMDD may experience intense irritability, sadness, anger, anxiety, trouble concentrating, low energy, suicidal thoughts and sometimes physical symptoms like joint pain, headaches, or bloating. These changes are not just frustrating, they can deeply affect work, relationships, and overall wellbeing.
Recent research shows that PMDD is caused by the brain's heightened sensitivity to normal hormone shifts, particularly to estrogen and progesterone. A 2023 study published in Biological Psychiatry found that brain regions responsible for regulating emotion respond differently in people with PMDD compared to those without. It's not a hormone imbalance—it's a neurobiological reaction to natural hormonal changes.
PMDD is real, cyclical, and diagnosable and yet often misunderstood or missed entirely. This blog is here to help change that.
This quiz is based on clinical criteria (DSM-5). The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition) is the standard classification system used by clinicians and researchers to diagnose and categorize mental health conditions.
Yes = 1 point
Not sure = 0.5 point
No = 0 points
Score Range Suggestion
0–2
Unlikely PMDD, but if something feels off, tracking could help.
3–5
Possible premenstrual mood disorder. Tracking and further support are recommended.
6–8
Strong indication of PMDD. We recommend to consult your doctor.
Many people, including healthcare professionals, mistakenly believe PMDD is caused by abnormal hormone levels. In reality, hormone levels in people with PMDD are typically within the normal range. The issue lies in how the brain responds to these hormonal shifts. This subtle but crucial distinction means that standard diagnostic tools, such as blood hormone tests, often fail to detect PMDD.
PMDD symptoms can mimic depression, anxiety, or bipolar disorder. Without tracking when symptoms occur in the cycle, the hormonal link is often missed. Many are misdiagnosed and prescribed treatments that don’t align with their cycle-based patterns, delaying proper care and causing a lot of unnecessary and unwanted side effects.
Healthcare systems often separate reproductive health and mental health. Gynecologists may overlook psychological distress; psychiatrists may not consider hormonal rhythms. As a result, PMDD gets stuck in the cracks, unseen, untreated.
Women's health, and especially menstrual mental health, has long been underfunded and under-researched. PMDD was only added to the DSM-5 in 2013, and medical education around it remains sparse. Gendered assumptions like “it’s just hormones” or “it’s PMS” often result in dismissal rather than support.
Because PMDD is cyclical, symptoms may appear and disappear without obvious cause unless tracked daily across multiple cycles. Without symptom diaries or validated tools like the DRSP (Daily Record of Severity of Problems), both patients and clinicians can miss the pattern entirely.
We’re advancing research and building future treatments grounded in scientific validation and lived experience. PMDD isn’t vague. It’s visible and it deserves scientific attention.
Our current drug development program is an oral, on-demand 3-MMC-based treatment to reduce both pain and severe mood swings. Early studies in a small patient group and healthy volunteers in collaboration with Maastricht University show promising results. These findings are especially relevant for PMDD, where both emotional and physical symptoms (like pain, tension, and discomfort) are significant and under-addressed. While we’ve just completed our Phase 1 clinical trial, we’re preparing for Phase 2 with cautious optimism and a deep commitment to scientific rigor.
Initial results from our research have been published in Nature and Psychopharmacology, supporting the neurobiological rationale for this compound’s relevance in cycle-related pain and mood modulation. Our work is further detailed in scientific papers led by Professor Johannes Ramaekers, who notes:
"We found that low doses of 3-MMC not only reduce pain perception but also interact with brain circuits relevant to mood regulation. This dual effect may offer a promising pathway for the treatment of disorders like PMDD that involve both emotional and physical symptoms."
As we've said before:
“PMDD isn’t just emotional, it’s also physical. And women deserve treatment options rooted in scientific prove, not dismissal.”
We give people the tools, language, and support to recognize what’s happening in their bodies. Through storytelling, cycle literacy, and community, we’re shifting the narrative from shame to shared understanding.
Together, we’re closing the awareness gap—and opening up new possibilities for healing.